KNEE, BALANCE, & WALKING
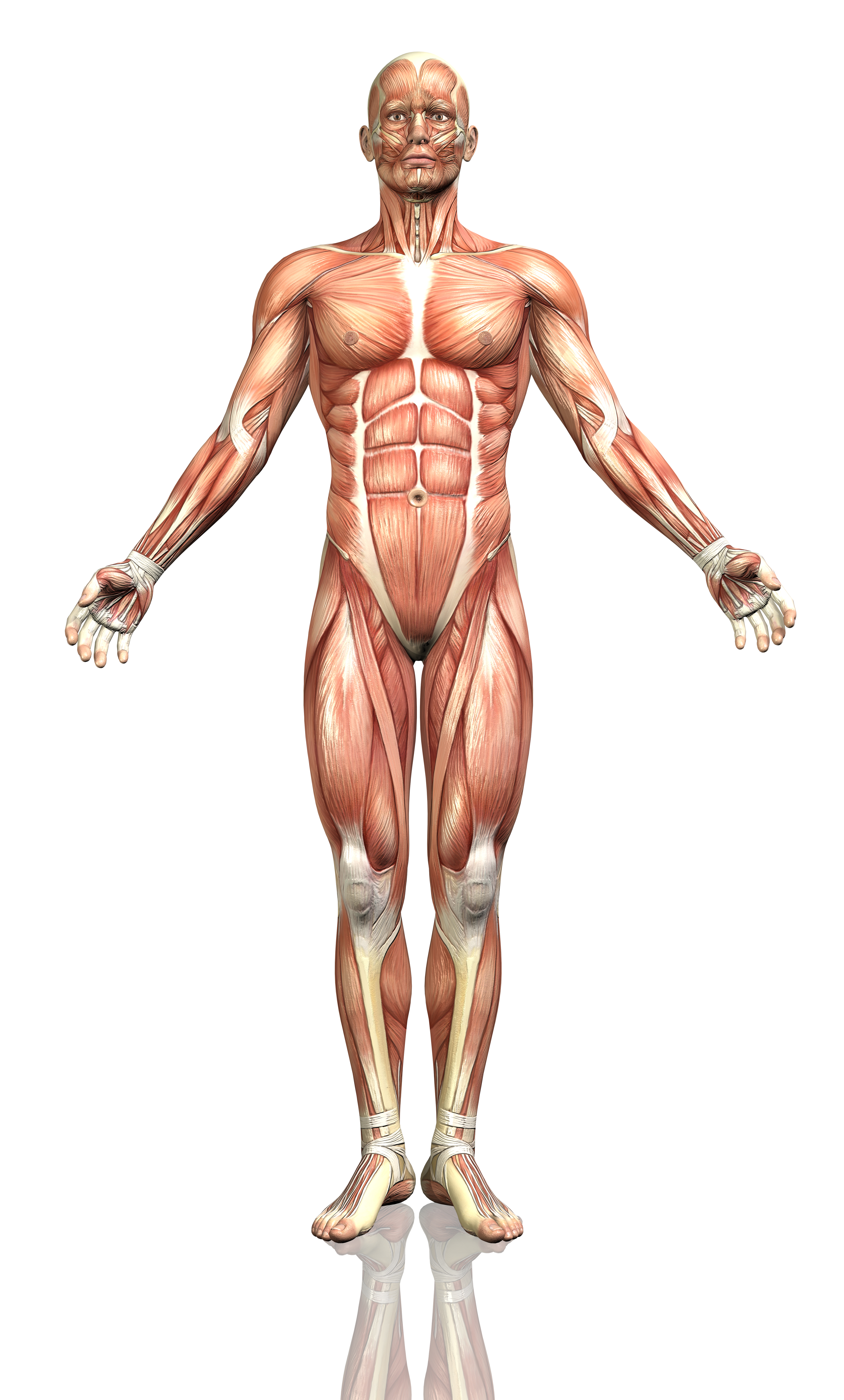
Display
Herniated or Bulging Disc of the Back/Lumbar Spine
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your back (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling to a specific part of the back, hips, legs, or feet. In more severe cases complete lack of sensation, muscle weakness, and paralysis of an area of the lower extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Our physical therapists will often use a McKenzie based treatment program to help centralize and abolish the symptoms. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Medial Cruciate Ligament (MCL) Tears
The medial cruciate ligament (MCL), is located along the inside of the knee, connecting the thigh bone (femur) to the shin bone (tibia). The role of the MCL is to provide stability to the inside of the knee against forces coming from the outside of the knee, as well as against forces rotating the lower leg outwards. Typically MCL injuries occur when the foot is planted on the ground and the knee is hit from the outside causing the knee to collapse inward.

How physical therapy helps
Our physical therapists are able to assess the MCL and determine the appropriate plan of care. If it is determine conservative treatment is appropriate, an individualized treatment program will be created that will address deficits that may include loss of range of motion, improve strength and stability, improve balance and proprioception, and resolve symptoms in order to return the individual to their prior level of activity and function.
Meniscus Injury
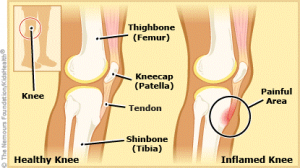
The meniscus is a ring of cartilage on the lower part of the knee (the tibial plateau) that the end of the large femur bone rides on. The meniscus is responsible for providing cushioning and stability of the knee joint while guiding movement. It is connected on the outer edges to the thick ligaments around the knee. The inside part of knee (medial meniscus) bears more weight and often sustains more damage than the outside part (lateral meniscus).

The meniscus is supposed to be smooth to ensure good gliding of the knee when it is bending. With injuries, poor alignment, or weak musculature, the meniscus can become bruised and even torn. The outside edges of the meniscus have more blood flow than the inner portions. This means, depending on the area were the damage is located, the healing process can be slow.
Many times, meniscus injuries are mild to moderate and can be rehabilitated with physical therapy. However, at times surgical intervention may be necessary to clean and shave down the torn areas of the meniscus. Physical therapy is very important in the full recovery after this surgical procedure.
How physical therapy helps
Physical therapy is a very important part of recovering from a meniscus injury. Most injuries are mild and involve small tears, bruising, or irritation. Physical therapy can pinpoint where there are limitations in movement of the knee joint and weakened musculature support. By pinpointing the mechanisms of injury, our treatments can focus on reducing your pain and swelling quickly. Then, we focus on improving your range of motion, joint mobility, and strengthening to make sure your meniscus receives the necessary support.
If surgery is necessary, we work closely with your physician and the rehabilitation protocol. The primary focus is on eliminating swelling quickly, resolving pain, improving range of motion, restoring normal walking, and strengthening the supporting muscles around the knee. We then show you what to do to maintain a healthy knee with physical activities and sports.
Tendonitis
The ending of the word “itis” is defined as inflammation. Therefore, tendonitis is inflammation of a tendon, which connects muscles to bones. Commonly, the tendon that connects your quadriceps muscle to the tibia bone (patella tendon) can become inflamed. This thick tendon runs over the top of your kneecap and attaches to the tibia bone below. This patella tendon can often become inflamed due to abnormal joint movements, poor posture, and weakness of the surrounding musculature. This causes strain to the tendon with resulting pain during repetitive movement and especially with squatting or kneeling down. Other areas of tendonitis in the knee can occur such as the back, outside, or inside of the knee.
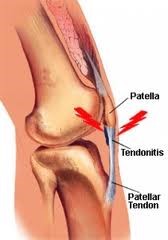
How physical therapy helps
Physical therapy is the first line in conservative treatment for tendonitis. Most tendonitis is due to underlying abnormal mechanics of movement, walking, and weakness. Our trained physical therapists are experts in evaluating your movement to pinpoint the source of the trouble. Modalities may be used to alleviate pain and discomfort, while hands-on therapy improves joint mechanics and movement.
Finally, strengthening exercises and joint coordination exercises help to restore stability to the affected area and prevent recurrence of symptoms.
Anterior Cruciate Ligament (ACL) Tears
The anterior cruciate ligament (ACL) is located within the knee joint and functionally works to stop the shin bone (tibia) from sliding forward on the thigh bone (femur) as well as restricting the knee from rotating in/out when the foot is not in contact with the ground. ACL injuries can be classified as either a contact injury or a non-contact injury. Contact injuries occur from either a direct impact to the knee or an impact to the body that changes the position of the knee. Non-contact ACL injuries occur from a sudden decelerating moment (i.e. planting, cutting, landing after a jump) with the knee extended and/or buckling inward.

How physical therapy helps
Our physical therapists are able to assess the ACL and determine the appropriate plan of care. If your physical therapist decides further examination is necessary, we will coordinate with your primary care provider. If it is determined conservative treatment is appropriate, an individualized treatment program will be created that will address deficits that may include loss of range of motion, improve strength and stability, improve balance and proprioception, and resolve symptoms in order to return the individual to their prior level of activity and function.
Posterior Cruciate Ligament (PCL) Tears
The posterior cruciate ligament (PCL) is an important ligament that checks the backward sliding of the tibia bone on the femur bone in the knee. This ligament can be injured with sports or falls, especially with blows to the front of the knee while the foot is planted on the ground.
The PCL can be sprained, which means it is still intact. If ruptured, it means it is completely broken. When a PCL injury involves a sprain, there is typically swelling that occurs in the knee and a feeling of instability with walking. Sprains are classified according to their severity with grades 1 through 3. Grades 1 and 2 are often treatable without surgery, while grade 3 is most often a complete tear and typically requires surgery.
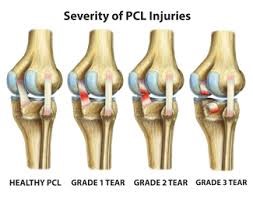
With a sprain, the ligament is overstretched and micro-tearing results, causing pain and inflammation. There is little blood flow to the ligaments, and they get most of their nutrition from the joint fluid. This means, that their healing is a lot slower than most other tissues. Depending on the severity of the sprain and joint stability, the potential for future injuries can increase.
With grade 3 PCL tears, surgery is most likely needed to repair. Physical therapy is vital to the rehabilitation after this surgery. Recovery does take time and the goal is to protect the surgery site, maintaining stability while getting back into walking and eventually running.
How physical therapy helps
Our physical therapists work with patients of all ages, especially those who have sustained PCL tears through sports activities. We work closely with your physician to examine the stability of your knee after the PCL injury. There are specific tests that we perform to assess how stable the ligament is and what course of action is best to resolve your pain and return you to activities as soon as possible. Most grade 1 and grade 2 sprains can be rehabilitated without the need for surgery, and our physical therapists will discuss your options.
If surgery is needed for your recovery, rest assured that you are in the right hands for your rehabilitation. We work closely with your physician’s rehabilitation protocols. The priority is to manage your pain and swelling after surgery, gradually increasing your range of motion in the knee per your post-surgery protocol.
As time progresses, we work with you to gain your strength back in the knee, improve stability of the joint, get you back to walking normally, and eventually back into advanced movements including running.
Lateral Cruciate Ligament (LCL) Tears
The lateral collateral ligament (LCL) is located along the outside of the knee joint, connecting the thigh bone (femur) to one of the lower leg bones (fibula). The LCL’s primary function is preventing the knee from buckling outwards. Injury to the LCL most often occurs when the foot is in contact with the ground and a force comes from the inside of the knee causing the knee to buckle outward.
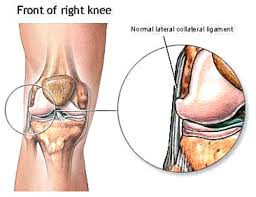
How physical therapy helps
Our physical therapists are able to assess the LCL and determine the appropriate plan of care. If your physical therapist decides further examination is necessary, we will coordinate with your primary care provider. If it is determined conservative treatment is appropriate, an individualized treatment program will be created that will address deficits that may include loss of range of motion, improve strength and stability, improve balance and proprioception, and resolve symptoms in order to return the individual to their prior level of activity and function.
display
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Total Knee Replacement
A total knee replacement surgery may be needed when the knee has suffered a significant trauma or due to severe arthritis. In a total knee replacement surgery, the ends of the femur and tibia bones, and backside of the kneecap are replaced. With a partial knee replacement, either the end of the femur bone or tibia is replaced. There have been many advancements in the technology of the total knee replacement prosthesis and procedures allowing for less invasive surgery and faster recovery times.
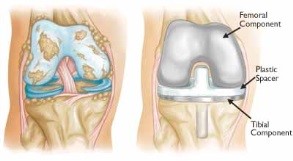
Typically, people have suffered for awhile before having surgery, leading to changes in walking, muscle strength, and function. Physical therapy before surgery, in general, has shown to help with the speed and quality of recovery after surgery.
How physical therapy helps
Working with your physician’s protocols, we coordinate a thorough rehabilitation program to get you back to normal walking as soon as possible . ypically, you start physical therapy in the hospital the day after your procedure. After progressing from the hospital, it is very important to continue with outpatient physical therapy.
We complete the rehabilitation cycle, further restoring your range of motion via your physician’s protocols, restoring normal walking, balance, knee coordination, and alleviating pain. We ensure that we continue to reinforce safety precautions with your knee movement while you heal. The end result is being able to return to most normal activities pain-free.
Poor Balance / Risk of Falling
Did you know that one out of three adults aged 65 and older fall each year? Among older adults, falls are the leading cause of both fatal and nonfatal injuries. Our ability to balance when walking or moving can change for a number of reasons. As we age, there is a natural loss of balance due to slowing down of reflexes, muscle weakness, and tissue changes. In addition, arthritis in the ankles, knees, or hips can affect balance. Furthermore, any neurological changes such as Parkinson’s Disease, Multiple Sclerosis, spinal cord injuries, nerve injuries, back problems, and much more can play a role in diminished balance.
Our ability to balance relies mainly on 3 factors. Our ability to perceive movement comes from the nerve sensors in our joints and muscles, our vision, and the position of our head in space through the vestibular system in the inner ear. When any one of these factors is not optimum, our ability to balance is affected and our risk for falling greatly increases.
People are often not aware of their change in balance as changes typically occur over a long period of time. A good rule of thumb to test your balance is being able to balance on one leg for 10 seconds without a problem. If you lose your balance quickly or wobble significantly, then you are at a higher fall risk.
The good news is that there is a lot than can easily be done to improve your ability to balance, which improves your walking and makes the risk of falling significantly less.
How physical therapy helps
Physical therapy is the main treatment for poor balance and reducing the risk of falls. It begins with a thorough evaluation of your walking, balance, coordination, joint movement, range of motion, and strength. In the case of neurological conditions, more testing is done to determine visual tracking and your vestibular system function, which contributes to your balance. (See our section of neurological conditions under the “Head” section on the body diagram for more specific information).
After discovering the root cause of your balance difficulties, we develop a treatment plan that will improve your ability to balance, walk, and negotiate uneven terrains such as grass, sand, stairs, and more. In addition, if you use a cane or walker, we can instruct you in the proper use of that adaptive equipment. Physical therapy goes a long way to improving your balance and setting you on the safe path to enjoying activities you love.
Sprain / Strain
Sprains refer to injuries of the ligaments (connect bone to bone), and strains refer to injuries of the muscles or tendons (connect muscle to bone). Sprains and strains occur from quick over-stretching of the tissues causing micro-tearing and subsequent injury. Swelling begins as part of the inflammation process, causing pain and difficulty with movement.
The first step in treating sprains or strains in the knee is to rest, ice, and elevate it. With severe limitations in movement, you should see our physical therapists right away. There are different levels of sprain or strain from mild to severe. In some cases, the tearing can be complete and even be in need of surgical repair.
How physical therapy helps
In most cases, physical therapy can effectively help you recover from a sprain or strain. We first evaluate the injured area to determine the extent of the injury and ensure that the ligaments or tendons are still intact. After we pinpoint the injured area, we formulate a treatment plan that will quickly relieve your swelling, pain, and begin restoring range of motion.
The goal of physical therapy is to restore your normal range of motion and eventually restore normal strength. If you participate in sports or are very active, we work closely with you to make sure that we help you fully recover and can participate in those activities you love to do.
Post-surgery Rehab
Knee Post-surgery Rehab
Other types of surgeries for the knee are fracture repairs or ligament/tissue repairs from trauma. The large amount of force it takes to break bone means that the soft tissues around the knee are most likely significantly injured also. After surgery, due to limited movement, range of motion is lost as well as strength. Since walking is a very complex action of different muscles moving in a coordinated fashion, it can be difficult to walk after a knee surgery.
How physical therapy helps
Physical therapy is an important part of the rehabilitative process after a knee surgery. Depending on your surgery and your physician’s protocols, we gently progress you through a structured rehabilitation program. The goal is to restore pain-free range of motion in the knee while maintaining surgery recovery protocols. Finally, walking coordination, balance, and strength are improved so you can return to normal pain-free walking.
Difficulty Walking
It takes us at least 12 months as a baby to learn the fundamentals of walking. It takes even longer to learn how to walk properly and eventually run. Walking is very complex and requires good balance, the ability to know where your joints are in space (proprioception), the ability to know how your joints are moving (kinesthesia), good range of motion, and strength.
As we age, with declining activity or after an injury, walking can become difficult. With pain in the knee or hip, our walking pattern can change, leaving us with a limp and possibly back pain. Changes in posture can also be responsible for changes in walking patterns.
When walking patterns change, abnormal stresses and strains with everyday activities can be transmitted to areas it shouldn’t. For example, if you have knee pain and you begin to limp, the other hip and your spine now have to take double the weight. This can lead to pain and dysfunction in those areas also. The good news is that walking can be helped, and our physical therapists are the experts uniquely trained to do so.
How physical therapy helps
One of the main specialties of physical therapy is helping people to walk normally. This takes a thorough evaluation of your range of motion, strength, walking patterns, balance, and coordination. By discovering in what area you have difficulties, we can paint a picture of why your walking is not as it should be.
We then coordinate an extensive, but easy to do, treatment plan that will address your range of motion, pain, coordination, balance, and strength. The end result is the ability to walk without the need of an assistive device such as a cane or walker, safely and smoothly.
Osgood Slatter’s Disease
Osgood-Schlatter Disease (OS) is considered an overuse injury that causes pain just below the knee joint and is typically the result of prolonged, excessive stress on the bone from rapid bone growth. During growth spurts, long bones may grow faster than what the surrounding muscle and tendon tissue can comfortably stretch. This results in a constant, increased level of tension where tendons attach the muscle to bones. The resulting irritation that occurs at the tendon-bone interface stimulates increased bone production which results in an enlargement of the bony bump (tibial tuberosity) on the upper shin bone (tibia) just below the knee cap (patella). Pain is often reported at this location, particularly with sports and activities requiring running, jumping, and cutting.
How physical therapy helps
Our physical therapists will perform a thorough, comprehensive examination and evaluation during which other conditions will be ruled out. Once a diagnosis of OS has been determined, a specific and individualized treatment plan will be created that focus on speeding your recover and returning you to your pain-free prior level of activity and function. There have been many forms of physical therapy treatments proven to be effective in treating OS, including range of motion, strengthening exercises, manual techniques, strategies for managing symptoms, functional training, and education.
Patellofemoral Pain Syndrome
Patellofemoral Pain Syndrome (PFPS)
Patellofemoral pain syndrome refers to pain at the front of the knee, in and around the kneecap. The pain usually is accompanied by tenderness along the edges of the patella.
Current research indicates that PFPS is an “overuse syndrome”, which means that it may result from repetitive or excessive use of the knee. Other causes may include: weakness, tightness, or stiffness in the muscles around the knee or an abnormality in the way the lower leg lines up with the hip, knee, and foot.
These conditions can interfere with the ability of the patella to glide smoothly on the femur (the bone that connects the knee to the thigh) during movement. The friction between the under-surface of the kneecap (patella) and the upper leg bone (femur) causes the pain and irritation commonly seen in PFPS. Usually, patellofemoral pain is worse when you walk up or down hills or stairs and on uneven surfaces. This pain tends to increase with activity and improve with rest. You also may feel pain after sitting for long periods of time with the knee bent or occasionally hear or feel a “cracking” or “popping” when you bend or straighten your knee.
How physical therapy helps
After an evaluation, our therapists will prescribe an exercise and rehabilitation program just for you. Your program may include strengthening and stretching exercises targeted at the hip, knee, and the ankle. Taping of the patella (kneecap) may be done to reduce pain and retrain muscles to work efficiently. Other treatments may include bracing, modalities such as electrical stimulation, and ice for pain.
If the alignment and position of your foot and arch appear to be contributing to your knee pain, our physical therapists may fit you with a special shoe insert called an orthosis. The orthosis can decrease the stress to your knee caused by excessive rotation or impact during walking and running.
Our physical therapists will work with you to help you stay active and maintain your fitness level. You may need to modify your activity level or change your training activities until you recover; however, our therapists will show you how to do activities and exercises that will not increase your pain. Most importantly, we’re happy to help make recommendations to help prevent PFPS from returning.
Ilio-tibial Band Syndrome (ITBS)
Iliotibial band syndrome (ITBS) occurs when excessive irritation causes pain on the outside (or lateral) part of the knee. The iliotibial band (ITB) is a type of soft tissue that runs along the side of the thigh from the pelvis to the knee. Irritation and inflammation arise from friction between the ITB and underlying structures when an individual moves through repetitive straightening (extension) and bending (flexion) of the knee. Typically, ITBS pain occurs with overuse during activities such as running and cycling.

How physical therapy helps
Physical therapy treatment often focuses on range of motion exercises for the hip and knee, as well as strengthening exercises to target the hip and core (abdominal) musculature. Manual hands-on therapy such as Astym may be performed to help decrease tightness to the area.
Knee Amputation (below-knee or above-knee)
Amputation (above-knee or below-knee)
Below-knee amputation (BKA) or Above-knee amputation (AKA) is a surgical procedure performed to remove the lower limb above or below the knee when that limb has been severely damaged or is diseased. Most amputations are performed due to peripheral vascular disease, or disease of the circulation in the lower limb. Poor circulation limits healing and immune responses to injury, and foot or leg ulcers may form and not heal. They may develop an infection, and it could spread to the bone becoming severe enough to be life-threatening. Amputation is performed to remove the diseased tissue and prevent the further spread of infection. If an amputation is necessary, it is usually performed by a vascular or orthopedic surgeon. The diseased or severely injured part of the limb will be removed, keeping as much of the healthy tissue and bone as possible. The surgeon shapes the remaining limb to allow the best use for a prosthetic leg after recovery.
How physical therapy helps
Physical therapists are often involved before the surgery to help start the patient on range of motion and strengthening exercises in preparation for surgery. Immediately following surgery, treatment is focused on range of motion exercises to decrease tightness as well as compression to manage swelling and start molding or shaping the limb in preparation for their new prosthetic leg. Pain management techniques such as ice, elevation, and massage can be used if needed. Our physical therapists work closely with the physician and prosthetist in the following weeks and months to progress the patient towards ambulation with their new prosthesis.
Knee Pain
The knee has to bear the weight of the body while moving through an incredible range of 130 degrees or more. When running the knee absorbs up to 6 times the weight of your body in force! In a lifetime, it is estimated that the average person will take over 216 million steps and walk 108,000 miles. With this amount of use, at times things can go wrong and lead to knee pain.
Most knee pain stems from the loss of what is called “accessory motions”. Accessory motions are the knee’s smaller movements that are sliding side-to-side, back and forth, as well as spinning and rotating. Without consistent stretching and especially without being very active, the tissues around the knee become tight. In addition, if the muscles in the front or back of the knee become weaker, that can lead to more abnormal forces on the knee joint.
All of these problems lead to increased friction and wear on the knee. The normal response is one of inflammation that can be felt as pain in and around the knee. A good rule of thumb is that if your pain is achy, a lack of normal joint fluid flow is occurring as well as possible decreased circulation around the knee to the muscles and tissues. However, with sharp pain during movement, an area in the knee is being severely pressed upon and the movement of the joint is not normal.
How physical therapy helps
Physical therapy is one of the most important treatments for knee pain. Whether it is from a sports injury, tight musculature, altered joint mechanics or arthritis, we can help!
The first step is to pinpoint the exact mechanism of why your knee pain is occurring. We perform a thorough evaluation of your posture, knee motion, knee and hip strength, walking analysis, and joint mobility. From this, we can discover the main reason for your knee pain and formulate a treatment plan that will alleviate it quickly.
Our physical therapists perform hands-on therapy to improve your knee joint mobility, reducing pain quickly. Modalities such as ultrasound may be used to reduce swelling and pain. Specific exercises will be performed to enhance your leg strength and address any unbalanced muscles that are contributing to your knee pain.
Pes Anserine Bursitis
The pes anserine bursa is a small, fluid-filled sac located 2–3 inches below the inner side of the knee. It lies beneath 3 tendons, and it prevents the tendons from rubbing on the shinbone of the lower leg. Bursitis means the bursa has become irritated and inflamed, and this condition is usually painful. Certain positions, motions, or disease processes can cause constant friction or stress on the bursa, leading to the development of bursitis.
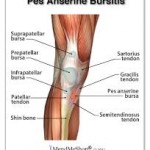
How physical therapy helps
The time it takes to heal this condition varies, but results can be achieved in 6-8 weeks or less when a proper stretching and strengthening program is implemented. Our physical therapists may use different types of treatments and technologies to control and reduce your pain and swelling including: ice, heat, ultrasound, electrical stimulation, taping, exercises, and manual therapy such as Astym treatment. Pes anserine bursitis is often related to tight hamstring muscles. Our physical therapists will determine if your hamstring muscles or any other leg muscles are tight and teach you how to stretch them properly.
Compartment Syndrome
Compartment syndrome is a serious medical condition that occurs when there is increased pressure in the muscular compartment of the limbs. Our limbs (arms and legs) are divided into compartments that contain different muscles, nerves, and blood vessels. Each compartment is separated by fascia, a thick sheet-like tissue that does not stretch. When there is excessive swelling within a compartment due to a severe acute injury or chronic overuse, pressure builds within that compartment as the fascia does not expand to accommodate the increased volume. In rare circumstances, this condition can be more than our bodies can handle, and the blood supply to the area is restricted. If the condition persists, the muscle and nerve tissue can be harmed. It is essential to relieve the pressure immediately to avoid permanent damage.
Compartment syndrome is classified as either acute or chronic. Acute compartment syndrome is a medical emergency, usually due to a traumatic injury, and must be addressed immediately to avoid irreversible consequences, such as limb loss. Chronic compartment syndrome develops over time, usually due to excessive or inefficient exercise exertion.
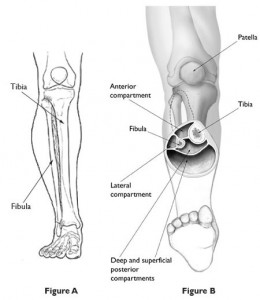
How physical therapy helps
Physical therapy can be effective to help identify the factors that may influence the development of compartment syndrome. Our physical therapists will often start with stretches to restore normal flexibility to the affected limb. Manual therapy, as well as Astym treatment, may be used to decrease tightness and restore normal muscle length and tone. Modalities such as ultrasound, iontophoresis, heat, or cold therapy may be used to decrease swelling. If symptoms don’t resolve or improve with preventative care, our therapists may refer you to an orthopedic specialist for potential surgical intervention.
