NECK
Display
Herniated or Bulging Disc of the Back/Lumbar Spine
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your back (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling to a specific part of the back, hips, legs, or feet. In more severe cases complete lack of sensation, muscle weakness, and paralysis of an area of the lower extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Our physical therapists will often use a McKenzie based treatment program to help centralize and abolish the symptoms. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Neck Pain
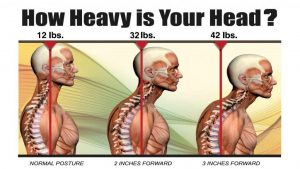
There are many different reasons for neck pain. The neck requires good alignment, proper movement, strength, and stability to work correctly. The neck or cervical spine has to bear the weight of the head, which is around 10-12 pounds (the weight of a bowling ball). With injury or prolonged poor posture (i.e. sitting at a computer), change in alignment, weakness, and instability start to occur. This irritates the structures of the neck and can even impinge on the nerves exiting the cervical spine or the central canal protecting the spinal cord.
How physical therapy helps
Our physical therapists perform a thorough evaluation of your neck to determine your range of motion, strength, posture, and alignment. Sometimes, where the pain is occurring, is not the source of the problem. Often, a limitation in movement above or below the painful area is causing excessive pressure or poor function of the painful area. We use gentle hands-on therapy, special exercises, and modalities such as ultrasound, electrical stimulation, or traction, to relieve your pain, restore motion, and get you back to activities quickly without neck pain.
Whiplash
Whiplash can occur with many different accidents, but is often seen in motor vehicle accidents. The weight of the head and spine is whipped back and forth with the fast movement of an accident or fall. The muscles in the neck don’t have time to react to the harsh forces, which can cause strain, rip, and tear of muscles, ligaments, and other tissues. In severe cases, fractures can occur in the bones of the neck (vertebrae).
Due to the shock and trauma initially from an accident, pain may or may not be present. Whiplash typically feels worse 1–2 days after the injury as inflammation sets in and tissues become swollen. This can lead to headaches, pain with movement, and even numbness/tingling into the upper extremities.
Often, people can have long-standing weakness of the neck muscles, leading to future problems, if their whiplash is not fully treated. Strengthening and postural exercises are very important to maintain stability in the neck after a whiplash injury.
How physical therapy helps
There are different phases or treatment to help you after suffering whiplash. Our physical therapists will determine the appropriate treatment to help you recover and relieve your pain. At first, very gentle hands-on therapy, massage, ultrasound, and electrical stimulation may be administered to relieve the pain and gently help swollen tissues recover. Gradual progression is then made with restoring range of motion and beginning very gentle exercises. As you progress and your pain reduces and range of motion improves, strengthening and postural exercises will be introduced to help you have a full recovery. It is very important to continue through with the recommended treatment plan our physical therapists provide to achieve a full recovery and prevent future problems from occurring.
Radiating pain
If you are experiencing radiating pain to the shoulder, shoulder blade, arms, or even your hands, the source of your trouble could be your neck or “cervical spine”. The nerves that supply sensation and movement travel from your neck down your arms. These nerves exit from your spine on both sides supplying the left and right sides, respectively. Often with poor posture, poor alignment, muscle weakness, or injury, the structure of the spine can change. This can lead to a narrowing of the holes where the different nerves exit from your spinal cord and out of the neck to the shoulders and upper extremities. These holes (foramen) depend on the proper alignment and movement of each level of joints in your neck.

Symptoms often start off as a mild, occasional tingling to certain areas of the shoulder, shoulder blade, arm, or hand. It can then worsen to pain and even numbness. Most symptoms can be reduced quickly. However, the time it takes to reduce symptoms depends on how long and to the extent the symptoms have been occurring. The sooner appropriate care and education is given, the quicker the recovery.
How physical therapy helps
Physical therapy is an important part of recovery from radiating shoulder, shoulder blade, arm, and hand pain. Our physical therapists work with you to determine the cause of the compression on the nerve structures. Often, there is a limitation in movement in the joints above or below the affected area of the neck. By improving neck joint mobility, posture, alignment, and muscle strength, support and stability can be returned to your neck. This reduces pressure on the affected nerve and allows it to heal, resolving symptoms.
Arthritis and Stenosis
Arthritis and Stenosis of the Neck/Cervical Spine
As we age, we use our neck joints and muscles thousands of times each day. This wear and tear over time can lead to bony changes in the joints and bones (vertebrae) of the neck. These bony changes, along with poor posture, cause spurs of bone that can rub and irritate the surrounding tissue.
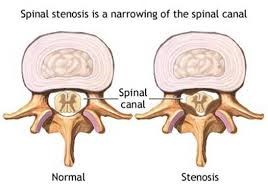
When the spurs protrude in the holes on the side of the neck where the nerves exit out (foramen), or the central spinal cord canal, this is called spinal stenosis. Spinal stenosis can be central stenosis or foramenal stenosis. It can cause a variety of symptoms ranging from chronic pain, to numbness and tingling into the arms. In severe cases of central canal stenosis (which affects the spinal cord), poor balance, pain in the legs, and difficulty with walking can occur.
People with osteoarthritis in the neck can experience chronic pain, stiffness, and limited range of motion with turning their head and looking up. Pain may be worse in the morning or after prolonged sitting.
People with rheumatoid arthritis can suffer with neck pain. It is very important for people with rheumatoid arthritis to maintain strength in their shoulders, neck, and postural muscles. This is because a very important ligament in the upper neck often weakens with rheumatoid arthritis and can be a serious health risk if injured.
How physical therapy helps
Physical therapy is very important for neck arthritis. Our physical therapists assess your range of motion, joint mobility, strength, and posture. From there, we determine the best plan of treatment, which may involve gentle hands-on therapy to restore joint range of motion, massage to improve muscle mobility, strengthening, range of motion exercises, and postural re–training. Our physical therapists work with you to restore natural movement, eliminate pain, and get you back to enjoying your normal activities.
Poor Posture and Forward Head/Rounded Shoulder Syndrome
Forward head/rounded shoulder syndrome is extremely common in today’s society and describes a condition where, due to changes in posture, the head juts forward causing actual shortening of the neck and the shoulders roll forward as well. This can be mild or severe and is affected by different factors such as type of work, age, arthritis, and genetic factors.
Due to prolonged sitting, poor posture with work, working at a computer, sitting at home in poor posture watching TV, and a host of other common poor postures, changes in your spine can occur over time. Think about how much time you spend looking into a screen and hunched over a desk. The 10–12 pounds of your head are pulling forward on your spine due to gravity. Over time, the normal curve in your neck reduces, the length of the spine decreases, and muscles in the neck become weaker. This can lead to a variety of symptoms from neck pain, to headaches, and even impinged nerves radiating pain into the upper extremities.
Physical therapy works in a variety of ways to improve your posture and actually change your neck posture over time. With hands-on therapy, stretching, special exercises, and postural re–training, our physical therapists work with you to improve your posture, alignment, and neck strength. In addition, we train you on proper postural positioning and techniques to adapt your work and home areas to reduce the strain on your neck.
Degenerative Disc Disease
Degenerative Disc Disease (DDD) and Degenerative Joint Disease (DJD)
As a normal part of the aging process, the fluid filled discs between our neck bones (vertebrae) dry out and shrink. However, in some individuals, this can be excessive, leading to a severe loss of height in one or more sections of the neck. This loss of height can increase rubbing of bone on bone, produce bone spurring, and increase pressure on joints and nerves exiting the neck. Symptoms can range from chronic aching pain in the neck, to radiating pain in the arms, numbness/tingling, and headaches.
How physical therapy helps
Physical therapy is a very important part in the maintenance of degenerative disc disease (DDD) and degenerative joint disease (DJD). While the disease process itself can’t be changed, maintaining good posture, joint mobility, alignment, strength, and range of motion can reduce or eliminate symptoms and maintain a healthier spine. Our physical therapists provide a great treatment solution to help you feel better and return to normal activities. If symptoms do return in the future, know that we are here to help you resolve your pain quickly.
display
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Herniated or Bulging Disc
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your neck (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, as well as poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling into a specific part of the shoulders, arms, or hands. In more severe cases, complete lack of sensation, muscle weakness, and paralysis of an area of the upper extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion as well. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Post-surgery Rehab
Neck/Cervical Spine Post-surgery Rehab
There are many different types of surgeries that are necessary for stabilizing the neck or cervical spine. Common surgeries include “cervical fusion” and “discectomy”. In a cervical fusion, one or more bones (vertebrae) are fused in the neck to stabilize the area. This may be due to fractures or for other reasons, such as the removal of a disc between the vertebrae “discectomy”.
How physical therapy helps
After surgery, our physical therapists work with you and your physician to follow a specific protocol of rehabilitation that reduces pain quickly, improves motion, increases strength, minimizes swelling, and returns you to activities as soon as possible.
Torticollis
Torticollis is the tilt and/or rotation of the head because of tight and weak neck muscles. It occurs when the muscle that runs up and toward the back of the neck (the sternocleidomastoid muscle) becomes tight, weakened, or thickened. The most common form is congenital muscular torticollis (CMT). It affects infants and is generally diagnosed within the first 2 months of life. CMT is often caused by birth trauma, or by sleeping or remaining in 1 position for a prolonged period of time.

How physical therapy helps
Regardless of the patient’s age, physical therapy is the primary treatment for all forms of torticollis. Our physical therapists provide treatment to address the impairments that are caused by torticollis. Early treatment results in the best outcomes.
Our physical therapists will work with a child’s caregiver or with an adult patient to develop and reach their goals. The primary focus is to instruct the parents/caregivers on a home stretching routine to regain normal neck range of motion, exercises to strengthen neck muscles, correct muscle imbalance, and improve the body’s alignment by easing muscle tension. These goals may be achieved through stretching, strengthening, massage, positioning, taping, and a home exercise program. If not treated, torticollis can become a permanent condition.
