FOOT AND ANKLE
Display
Herniated or Bulging Disc of the Back/Lumbar Spine
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your back (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling to a specific part of the back, hips, legs, or feet. In more severe cases complete lack of sensation, muscle weakness, and paralysis of an area of the lower extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Our physical therapists will often use a McKenzie based treatment program to help centralize and abolish the symptoms. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Achilles Tendonitis
Achilles tendonitis is an inflammation of the Achilles tendon that attaches your calf muscle to the back of your heel. Achilles tendonitis is typically caused by tightness in the hamstrings and calf muscles. In addition, limitations in ankle and foot range of motion can alter your walking pattern, putting excessive strain on the Achilles tendon, causing tendonitis.

Typically, the back of the ankle and heel is very painful to touch, especially after prolonged walking. Rest tends to help Achilles tendonitis, while walking aggravates it.
How physical therapy helps
Physical therapy is one of the best treatment options for Achilles tendonitis. Our physical therapists will evaluate your leg, ankle, and foot mobility, range of motion, strength, balance, and walking patterns. This will help us discover the root cause of your pain and resolve that for long-term results.
We focus on treatments to resolve your pain quickly, improve your joint mobility, and strengthen muscles as needed. The result is the ability to walk and run without pain in the back of your heel and returning to the activities you love to do.
Sprain / Strain
Foot/Ankle Sprain / Strain
A sprain in the foot/ankle involves the ligaments, and a strain involves the muscles around the foot/ankle. A sprain/strain typically occurs because the tissue has been overstretched too quickly, resulting in micro-tearing of the tissue. This results in painful inflammation, typically increased with movement and use of the damaged tissue.
The damage from a sprain/strain can be minor or major, depending on the severity of the injury, person’s health, and age. As we age, our tissue becomes less elastic and becomes more prone to tearing.
How physical therapy helps
Physical therapy is a very important part of the recovery from a sprain/strain. First the focus is on reducing pain and inflammation while maintaining or regaining range of motion. After the inflammatory phase is coming to an end, the focus shifts to attaining full range of motion then gradual strengthening of the injured areas to regain normal strength. Towards the end of treatment, focus is shifted to the coordination/balance of the foot/ankle joint and education towards preventing future injury. If you have suffered a sprain or strain, we’ll see you as soon as possible to start feeling relief and getting back to normal activities.
Fractures
Fractures in the foot/ankle occur for a variety of reasons. Fractures can occur in seniors also due to osteoporosis (thinning and weakening of bone).
The goal with fracture management is to provide a safe position for the bone heal (typically around 8 weeks), while maintaining range of motion. As the bone heals, strengthening can begin and rehabilitation back to normal activities is progressed.
At times, surgery may be needed to hold the bone together with plates or screws. This stabilizes the bone, but does disrupt muscles and leads to more weakness in the foot and leg muscles. Physical therapy is very much needed after this to restore normal range of motion and strength to the lower extremity. Recovery times can vary, but traditionally take 12–16 weeks.
How physical therapy helps
Physical therapy is a very important part of rehabilitation after a foot/ankle fracture. Whether you are a young person or older, we work closely with you and your physician to make sure your fracture is protected while it heals. We then work closely with you to gradually restore your range of motion, relieve pain, soothe aching muscles, and improve your strength.
The goal of physical therapy is to return you to normal activities after the normal course of bone healing. We can prevent long-term damage and address any issues that may have caused it in the first place.
Instability
Ankle Instability
Ankle instability typically occurs after the ligaments in the ankle have stretched out, losing the normal stability of the bones in the ankle and foot. This can be a result of an injury or occur over a long period of time from poor foot positioning, bad shoe wear, or genetic predisposition.
When there is ankle instability, the probability of further ankle sprains increases significantly. While the ligaments themselves may not be able to shorten back to normal, the muscles supporting the ankle can be strengthened to take up the slack. This compensation allows for better stability in the ankle and foot with walking, running, and sports. Bracing may also be needed depending on the severity of the instability.
How physical therapy helps
Our physical therapists work with different physicians, including podiatrists, to rehabilitate ankle and foot injuries. By assessing your ankle and foot joint movements, we can determine what areas need to be strengthened, bringing support and stability to your ankle. With years of training in analyzing and treating joint mechanics, as well as walking and movement, we put together a custom treatment plan that will improve your ankle stability.
Plantar Fasciitis
Plantar fasciitis refers to inflammation of the plantar fascia, which is a thick band of tissue on the underside of the foot, connecting from the heel to the ball of the foot. Plantar fasciitis typically occurs from tightening of the tissues under the foot and even further up in the legs. In addition, changes in the shape of the foot, such as fallen arches or changes in shoe wear can affect plantar fasciitis. Furthermore, with changes in walking posture for a variety of reasons, the strain on the plantar fascia can increase significantly.
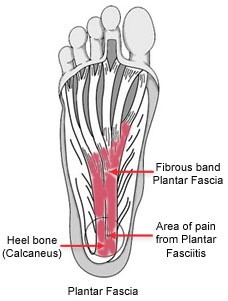
Plantar fasciitis is commonly felt as burning or sharp pain when standing on the affected leg. This typically occurs first thing in the morning or with initial standing after sitting for a prolonged period. Inflammation builds up during the day in the fascia, and may begin to hurt after prolonged walking. As you sit or sleep the inflammation thickens and the plantar fascia stiffens. When you go to step on the foot, the inflamed and stiff tissue stretches causing pain. Pain may be felt mostly in the heel, but can extend along the bottom of the foot.
How physical therapy helps
Physical therapy is very beneficial in treating plantar fasciitis. At first we evaluate your movement, posture, walking pattern, and ankle/foot mobility. Our hands-on therapy is great for soothing the irritated tissue in the foot and also improving range of motion in the foot and ankle joints. Astym may be used to help restore normal tissue integrity and decrease areas of tightness. Modalities, such as ultrasound and ice, may be used to reduce swelling and pain quickly. Supportive shoes/orthotics may be recommended as well as night splints. Our goal is to reduce your pain quickly and strengthen your feet for long-term results.
Heel spurs
Heel spurs are a bony growth that form on the heel bone. Heel spurs can occur by themselves or they may occur along with plantar fasciitis. 1 out of 10 people have heel spurs, but only 5% of people with heel spurs have foot pain. Because the spur is not the cause of plantar fasciitis, the pain can be treated without removing the spur.

How physical therapy helps
If x-rays reveal a bone spur and you are having pain with it, it is commonly treated very similar to that of plantar fasciitis. Treatment may include ice, anti-inflammatory medications, gastroc/soleus stretches, Astym, as well as the use of supportive shoes/orthotics may be recommended.
display
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Posterior Tibialis Tendonitis
Posterior tibialis tendon dysfunction (PTTD) is caused by degeneration of the posterior tibialis tendon, which starts in the calf, runs behind and below the boney protrusion of the inside ankle, and ends on bones in the middle of the foot. Because of the tendon’s location, it is able to help support one of the major arches of the foot. People with this problem have pain and swelling in the ankle and foot, especially with activity; are flatfooted; and can’t stand on their toes. Risk factors for developing this problem includes wearing poorly fitting footwear, changes in the arches of the feet, age, obesity, diabetes, or prolonged activity like walking or jogging.

How physical therapy helps
Our physical therapists will evaluate your feet and help to identify the root cause of the PTTD, as well as develop an appropriate plan of care to eliminate pain and restore normal function of the foot. Your treatment plan may include exercises for stretching and strengthening of the lower leg and foot intrinsic muscles. Other treatment may include manual therapy , joint and soft tissue mobilization, an orthotic to support the arches in the foot, and recommendations about footwear that is appropriate for your foot type.
Morton's Neuroma
Morton’s neuroma is an injury to the nerve between the toes, which causes thickening and pain. It commonly affects the nerve that travels between the third and fourth toes. The exact cause is unknown. Doctors believe the following may play a role in the development of this condition: wearing tight shoes and high heels, abnormal positioning of toes, flat feet, forefoot problems including bunions and hammer toes, and high foot arches. Morton’s neuroma is more common in women than in men.

How physical therapy helps
Physical therapy is often the first line of treatment for this condition, and it is vitally important that it is given focused, dedicated attention. We often can treat the pain without the need to resort to more complicated methods. Even when other methods, such as medications and surgeries, are used, physical therapy is an important adjunct to help healing and reducing the pain.
The types of physical therapy that are used for Morton’s neuroma include:
- Stretching and Massage: this helps increase the flexibility of the affected area by loosening tight tendons and ligaments.
- Toe Exercises: muscle strengthening through toe exercises is an important part of physical therapy to minimize the effect of Morton’s neuroma.
- Ankle Exercises: as a result of the pain from Morton’s neuroma, the muscles that support your ankle can become weak. Strengthening exercises can strengthen the ankle, providing more stability and lessen the chances of further injury.
Total Ankle Replacement
Total ankle arthroplasty (TAA), also known as total ankle replacement, is a surgical procedure that orthopedic foot and ankle surgeons use to treat ankle arthritis. Arthritic changes may be a result of normal wear and tear due to aging or from an injury such as a broken ankle or dislocation. Arthritis eventually leads to loss of cartilage, pain, and/or deformity. The goal of TAA is to improve ankle motion so the patient has less pain during activity. TAA is considered in patients that experience ankle pain and decreased function from arthritis after trying conservative management such as anti-inflammatory and pain medications, bracing, physical therapy, and activity modifications. Patients with rheumatoid arthritis are usually good candidates for the ankle joint replacement. Other patients that should be considered are those that need but do not want a fusion-type procedure that would eliminate the motion at the ankle joint.

How physical therapy helps
Recovery from a total ankle replacement requires a period of non-weightbearing and immobilization. Our physical therapists follow a strict protocol from the physician for regaining normal range of motion, strength, and balance for a full recovery.
Shin Splints
Shin Splints is a condition that causes pain on the inside of the shin (the front part of the leg between the knee and ankle). It is one of the most common athletic injuries. It affects both the muscle on the inside of the shin and the bone to which it attaches. Shin splints may affect up to 35% of athletes who run and jump, such as distance runners, sprinters, basketball or tennis players, or gymnasts. Military personnel, dancers, and other active people can also develop it. Physical therapy can help you recover from shin splints and teach you exercises and tactics to prevent re-injury.

How physical therapy helps
Our physical therapists commonly treat shin splints with a variety of methods including the following: proper stretching and strengthening exercises to restore normal range of motion, manual therapy including Astym or massage to decrease tightness, and modalities including ice and ultrasound to help decrease pain. Some patients benefit from taping techniques of the leg or foot/arch to help improve mechanics and decrease pain with activity.
Compartment Syndrome
Our limbs (arms and legs) are divided into compartments that contain different muscles, nerves, and blood vessels. Each compartment is separated by fascia, a thick sheet-like tissue that does not stretch.
Our bodies are able to handle small changes in the pressure levels within these compartments. For example, our tissues may swell slightly after a hard workout or a mild injury. However, when there is excessive swelling within a compartment due to a severe acute injury or chronic overuse, pressure builds within that compartment as the fascia does not expand to accommodate the increased volume. In rare circumstances, this condition can be more than our bodies can handle, and the blood supply to the area is restricted. If the condition persists, the muscle and nerve tissue can be harmed. It is essential to relieve the pressure immediately to avoid permanent damage.
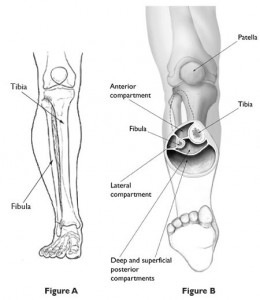
How physical therapy helps
Because the symptoms of Compartment Syndrome are similar to many other conditions, it is important that a physician or physical therapist rules out other possible diagnoses, such as tendonitis, stress fractures, shin splints, or other inflammatory conditions. The examination may include the use of diagnostic imaging, such as an ultrasound, x-ray, or MRI to assess the tissues in the painful area.
If Compartment Syndrome is suspected, an individual will likely be referred to a physician for a specific test called the “compartment pressure measurement”. This test is only used in cases where it is strongly suspected. This test is performed in a medical office. If Compartment Syndrome is diagnosed, your medical team will devise a plan to best treat your specific condition. For more mild cases of Compartment Syndrome, you will likely be referred directly to physical therapy. At our clinics, treatment will focus on range of motion, strengthening, and stretching exercises to restore normal movement and strength. Modalities including ultrasound, heat, or ice and manual therapy are used to decrease pain and tightness. In more severe cases, individuals are likely to be referred to a surgeon to discuss the option of a fasciotomy.
Turf Toe
Turf toe is an injury to the main joint of the big toe. The formal medical name for the condition is metatarsophalangeal (MTP) joint sprain. This injury occurs when the big toe is forced into extreme positions of hyperextension (where the toe moves back toward the top of the foot past its normal range of motion). It occurs primarily in athletic environments, particularly in football, when an athlete pushes off to sprint or is tackled with the front of the foot fixed and jammed into the ground, causing the toe to get stuck or caught in a hyperextended position. In most circumstances, a turf toe injury does not require surgery and can be treated effectively by our physical therapists.

How physical therapy helps
Immediately following a turf toe injury, the RICE protocol is recommended: Rest, Ice, Compression, and Elevation. The goal of the RICE protocol is to decrease pain and swelling and protect the joint from further injury until it can be more thoroughly assessed. Most turf toe injuries do not require surgery and are treated with physical therapy. The treatment depends on the severity of the injury.
- Grade 1: To treat a Grade 1 injury, our physical therapists may use narrow athletic tape to immobilize your big toe with your second toe to restrict painful motion. They may also place a firm insert in your shoe to limit motion and promote healing. In many cases, an athlete may be able to return to sport soon after a Grade 1 injury.
- Grade 2: Treating Grade 2 injuries may require immobilizing the foot in a brace or walking boot, and allowing several days/weeks of rest.
- Grade 3: Treatment of Grade 3 injuries is dependent on the severity of the damage to the structures of the foot. Surgery may be required if there is a fracture of a bone, damage to the cartilage (the tissue that lines the bones of the joints), a complete tearing of the tendon, or excessive movement of the joint that causes repetitive instability (subluxation or dislocation).
In each case, our physical therapists will work with you to design an individualized treatment program specific to the exact nature of your condition and your goals.
Post-surgery Rehab
Foot Post-surgery Rehab
Other types of surgeries for the ankle are fracture repairs or ligament/tissue repair from trauma. The large amount of force it takes to break bone means that the soft tissues around the foot are most likely significantly injured also. After surgery, due to limited movement, range of motion is lost as well as strength. Since walking is a very complex action of different muscles moving in a coordinated fashion, it can be difficult to walk after an ankle or foot surgery.
How physical therapy helps
After surgery, our physical therapists work with you and your physician to follow a specific protocol of rehabilitation that reduces pain quickly, improves motion, increases strength, minimizes swelling, and returns you to activities as soon as possible.
Bunions
A bunion (hallux valgus) is a large bump on the side of the foot that develops at the base of the big toe. It is common for a bunion to become inflamed and swollen, causing foot pain. Although anyone can develop a bunion, the condition most often occurs in women and older adults. Over time, the joint may enlarge and become stiff and painful, causing problems with shoe fitting, pain, and difficulty walking. A bunion is classified as mild, moderate, large, or severe, depending on the size of the measured angle at the toe. An angle of 20° or greater is considered abnormal.

Several factors that may cause bunions include:
- Heredity
- How the
- foot is shaped
- Flat arches
- Joint laxity (too much flexibility in the joint at the base of the big toe)
- Osteoarthritis
Tight footwear has often been blamed for bunions, but recent research suggests that footwear may not be a factor in their development. However, tight footwear can irritate a bunion by rubbing on the tissue at the joint, creating more swelling and pain.
How physical therapy helps
Our physical therapists will treat your bunion symptoms with pain management, exercise, gait training, and education regarding proper footwear and self-care for symptom management. The goal of physical therapy treatment is to improve the angle of the big toe, improve muscle strength, and reduce pain. Our physical therapists may also apply specialized taping of the big toe to improve the big toe’s alignment and reduce pain. We will recommend the best footwear for your condition as well. In some cases, we may recommend the use of splints, foot orthotics, or assistive devices, depending on your condition, and will train you in their use. They may include:
- Splints and toe separators to reduce pain and pressure on the big toe.
- Custom arch supports (foot orthotics) to help keep the foot and ankle in a mid-line position during walking.
- A cane, walker, or crutches (assistive devices) to reduce pain and improve walking ability.
Stress Fracture
Stress fractures are tiny cracks that occur in bone, usually related to repetitive activities that impact the bone in a similar way over time. These stresses lead to change in the normal process of bone breakdown and reformation. Stress fractures are most common in the feet and legs as these structures bear weight during walking, running, and jumping. Lower extremity stress fractures are a relatively common injury seen most often in athletes playing sports that require repetitive impacts (running and jumping). Stress fractures make up about 8% of all activity-related injuries of the lower extremities. Female athletes are about one-third more likely to develop stress fractures in the legs and feet. While athletes may be more susceptible to these types of injuries, individuals who walk, march, or spend much of their workday on hard floors are also at risk.
How physical therapy helps
Our physical therapists can help with recovery after a stress fracture, as well as identify potential risk factors for prevention of future stress fractures. Stress fractures are treated by resting the leg as much as possible. Whatever activities you are participating in that increase force in the legs (running, jumping, or “cutting” in sports) must be stopped for at least 3 weeks in order for the bone to begin the healing process. Our physical therapists can decide whether you should use a compressive brace, crutches, or a walking boot to protect your bone while it is healing as well.
We can design a specific treatment program for you to follow at home to help speed up your recovery. Initial treatment will focus on muscle-strengthening exercises using bands rather than heavy weights. Other treatment may include:
- Range-of-motion exercises: Since you have been less mobile over the past few weeks, your range of motion may have decreased. Our physical therapists will teach you how to perform safe and effective exercises to restore full movement in the joints of your legs.
- Muscle-strengthening exercises: Even short-term inactivity weakens the muscles of the legs, increasing the potential for new injuries. Additionally, your stress fracture may have been related to some underlying weakness in the legs. We can determine which strengthening exercises are right for you based on the severity of your injury and where you are in your recovery.
- Body awareness and balance training: Specialized training exercises help your muscles “learn” to respond to changes in your environment, such as uneven or unstable surfaces. When you are able to put full weight on your foot without pain, our physical therapists may prescribe these exercises to help you return to your normal activities. For instance, you might learn how to stand on 1 leg or stand on a wobble board, with or without your eyes closed, to challenge the muscles in your legs.
- Functional training: When you can walk freely without pain, our physical therapists may begin “progressing” your treatment program to include activities that you were doing before your injury. This program will begin with slow and progressive weightbearing activities, such as hopping and light jogging. We will create your own unique training program, based on the examination of your legs, your goals, and your activity level and general health.
