HEAD
Display
Herniated or Bulging Disc of the Back/Lumbar Spine
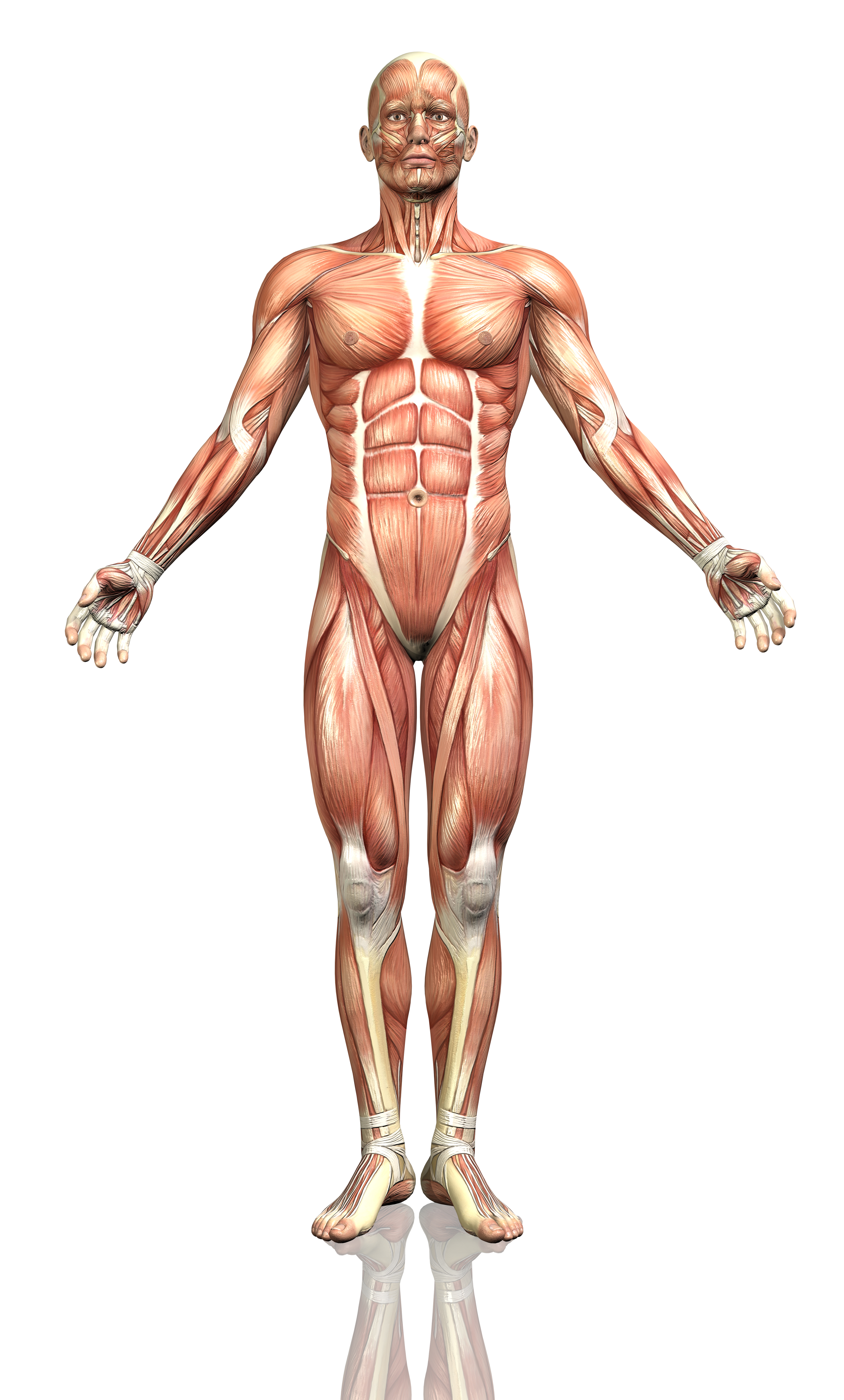
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your back (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling to a specific part of the back, hips, legs, or feet. In more severe cases complete lack of sensation, muscle weakness, and paralysis of an area of the lower extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Our physical therapists will often use a McKenzie based treatment program to help centralize and abolish the symptoms. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Headaches and Migraines
Over 45 million Americans suffer from headaches. There are many different types of headaches and migraines from tension headaches, temporal headaches, cluster headaches, migraines, and sinus headaches. While there are many different “triggers” such as alcohol, chocolate, scents, and other factors for headaches and migraines, most sufferers do have some underlying neck problem that causes their headaches. These are called “cervico-genic headaches”.
Headaches and migraines are often spasms/muscle tightness at the base of the neck triggering a whirlwind of abnormal electrical activity in the brain. This can cause a variety of symptoms depending on where this is occurring in the head. Most headaches have a component of stress. When stressed, our neck muscles tense on a chronic basis, and with supporting our head all day long, become very irritated. Along with other triggers, this can start a headache or migraine. It is why many headache and migraine sufferers have symptoms later on in the day.
How physical therapy helps
Our trained physical therapists examine many different factors that can be adding to the causes of your headache or migraine. They look for correct alignment and posture, muscle strength of the neck, upper back and shoulders, as well as joint movement in the neck and much more.
If there are limitations in movement or weakness in the neck or upper back, this will be addressed to restore your normal mobility. This also increases blood flow in the area, reducing the common spasms that can occur. In addition, our physical therapists will train you on exercises and techniques that you can use to prevent future occurrences.
Temporomandibular Joint Dysfunction (TMD or TMJ)
Temporomandibular Joint Dysfunction (TMD) describes the problems that may occur at the temporomandibular joint (TMJ). This joint is where your jaw bone attaches to the skull. It is a complex joint that has to slide forward and drop down in order for your jaw to open. It moves thousands of times a day with talking, eating, and any time you move your jaw. The joint has a disc or fluid filled sac within it and has many ligaments and muscles that coordinate movements.
The TMJ relies heavily on proper posture and alignment to function well. The posture and positioning of the neck and head play a large role in the pulls of muscles on the TMJ. Abnormal muscle pulls can lead to altered movement of the TMJ and thus pain.
How physical therapy helps
Physical therapy helps TMJ sufferers in a number of ways. Our physical therapists work with you to determine the exact mechanisms of your TMJ and where you have poor alignment of the TMJ, neck, and head. By improving posture, as well as movement and function, the normal muscle balance and movement of the TMJ can be restored. Specific exercises of the mouth/jaw are often given to help decrease amount of clicking/locking of the joint.
Vertigo and Dizziness
Vertigo
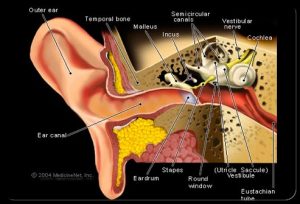
Vertigo and dizziness can be the result of a variety of different factors. Vertigo or benign paroxysmal positional vertigo (BPPV) can occur because of calcium crystals that form in the inner ear labyrinth canals. These canals give feedback about balance to your brain.
Dizziness
Dizziness can occur for a variety of reasons, including issues with medication. Issues with mobility of the neck joints and muscles can also affect dizziness. When this occurs, the major arteries in the neck that supply the back portion of the brain that control balance and orientation can be affected.
How physical therapy helps
Our physical therapists perform a thorough examination of your balance and vestibular symptoms. We evaluate your visual movements, positioning of your head, neck mobility, and balance. At times, we may need to provoke symptoms to determine the exact mechanism of your vertigo or dizziness.
If you are suffering with dizziness and vertigo, you can benefit from physical therapy intervention to improve symptoms and increase your neck mobility. There are specific vestibular and balance exercises that are performed to settle the calcium deposits in the inner ear and improve your balance systems. Often times, symptoms are fully resolved within 1-2 treatments.
Concussion
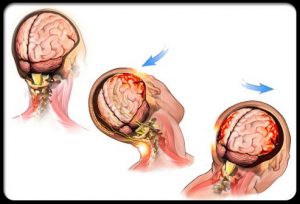
A concussion is a brain injury, often called a mild traumatic brain injury (mTBI), that is caused by either a direct blow to the head, face, neck, or body that transmits an impulsive force to the brain. The resulting impact between the brain and the skull results in altered functioning of the brain and symptoms that commonly include headache, feeling of fogginess, changes in emotional state, light and sound sensitivity, confusion, fatigue, nausea or vomiting, and difficulty concentrating. While these symptoms are typically short-lived and resolve spontaneously, there can be more serious conditions that occur and therefore all concussions should be assessed and managed by a trained medical professional.
How physical therapy helps
In the state of Iowa, physical therapists are one of the medical professional that are authorized to assess and manage individuals who have had a concussion. Our physical therapists will perform a thorough and comprehensive examination and evaluation which will then be used in forming an individualized treatment plan to safely return the individual to their prior status. As with any muscle, tendon, or ligament injury, healing tissue needs to have a graded progression of activities to heal properly and the brain is no different. Current research suggests a multi-step progression that reintroduces different forms and degrees of stimulus to the brain and is progressed based upon the individual’s symptom response. Our trained physical therapists are able to take patient’s through this progression to ensure the best and safest outcome, whether that be to return to sport, work, or just enjoying life.
TBI (Traumatic Brain Injury)
Traumatic brain injury (TBI) occurs as the result of extreme force exerted on brain tissue. Common causes are a bump, blow, or jolt to the head or a penetrating head injury that disrupts the normal function of the brain. Not all blows or jolts to the head result in a TBI. The severity of a TBI may range from “mild” (i.e. a brief change in mental status or consciousness) to “severe” (i.e. an extended period of unconsciousness or memory loss after the injury). Most TBIs that occur each year are mild, commonly called concussions.
How physical therapy helps
Physical therapists help people with TBI regain their physical abilities, re-learn daily tasks, and improve their strength and overall fitness. By working with the patient and his or her family, goals are developed to improve physical independence. Physical therapists help patients with TBI regain functions such as getting in and out of bed and changing their position in bed, sitting down, rising to stand, walking, and using a wheelchair. Our physical therapists use exercise and task-specific training to help patients improve alertness, flexibility, balance, strength, coordination, as well as return to sport/fitness activities and activities of daily living. They may also help with administering braces and/or assistive equipment when needed.
Bell’s Palsy
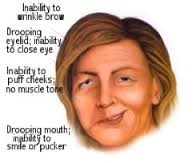
Bell’s palsy is a form of temporary facial paralysis. It occurs when the nerve that controls movement on one side of your face becomes inflamed. The condition often comes on suddenly but improves on its own within a few weeks. Although the cause of Bell’s palsy remains unclear, it’s thought that some cases might be caused by the herpes virus that also causes cold sores. Bell’s palsy usually begins with a sudden weakness on one side of your face or a sudden feeling that you can’t move one side of your face. The weakness gets worse quickly. Other symptoms include inability to close the eye on the affected side, drooping of the affected side (within a few hours to overnight), teary-ness/dryness of the eye, pain in or behind your ear, sensitivity to sound, drooling, and loss of sense of taste.
 How physical therapy helps
How physical therapy helps
At your first physical therapy appointment, our physical therapists will evaluate your condition and conduct a physical exam. After this is completed, the therapist will educate you about how to protect your face and your eyes, show you how to manage your daily life functions while you have facial paralysis, as well as explain the expected path to recovery. You will be given a home exercise program designed to restore your facial muscle activity to a normal state. Occasionally, modalities will be used to facilitate normal muscle activity. Finally, they will evaluate your progress and determine whether you need to be referred to a specialist if progress is not being made.
display
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
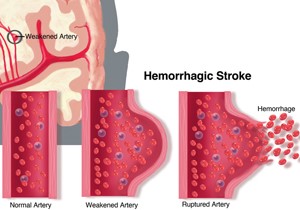
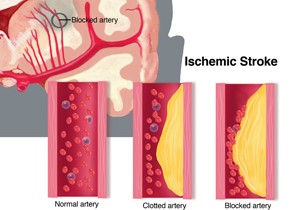
Stroke
A stroke is sometimes called a “brain attack”. With a heart attack, blood supply to the heart is reduced or stopped. With a stroke, blood supply to part of the brain is reduced or stopped. This means that part of the brain does not receive enough oxygen. Millions of brain cells die every minute during a stroke, increasing the risk of permanent brain damage, disability, or death. One common cause of blockage that leads to a stroke is a blood clot or a build-up of fatty deposits (arteriosclerosis) in blood vessels that supply the brain. The reduction in blood flow results in an ischemic stroke. Most strokes are ischemic. Another common cause of a stroke is a leaking vessel in the brain. This is called a hemorrhagic stroke.
How physical therapy helps
How well you recover from a stroke, and how long it takes to recover, depends on the size and location of the stroke, how quickly you receive care, and in some cases, other health conditions you might already have.
Rehabilitation begins very soon after your stroke, and physical therapy is an important component of your health care team. Physical therapy’s main goal is to help you return to your roles in the home, in the community, and at work.
After examining you and evaluating your condition, our physical therapists will develop an individualized plan to help you achieve the best quality of life you can. The plan will focus on your ability to move, any pain you might have, and ways to prevent problems that can occur after a stroke.
One of the first things our physical therapists will do is show you how to move safely from the bed to a chair. Later, the therapist will:
- Help you relearn how to walk
- Fit you with a wheelchair, if needed
- Provide training to your family and caregivers
- Train you in how to use devices that can help you keep mobile when a stroke has affected your ability to move, walk, or keep your balance: orthoses, prostheses, canes, walkers, wheelchairs—perhaps even robotics.
Depending on the results of the physical therapist’s evaluation, and depending on how long it’s been since you had your stroke, treatment will vary. In our outpatient setting here, the primary focus is on restoring your normal function of walking and balance to decrease your risk for falling.
Parkinson’s Disease
Parkinson’s disease (PD) is related to a loss of nerve cells in your brain that produce a chemical called dopamine. Dopamine is an important factor in controlling movement. The exact cause of PD is not yet known; however, family history, aging, or exposure to certain environmental toxins may contribute to the onset of PD. It is a chronic degenerative disease, which means that it gets worse over time. However, people usually do not die from PD.
The severity and type of symptoms of PD can vary widely. Some people have the disease for 20 to 30 years and have a slower progression and decline in mobility over a long period of time. For others, the disease progresses more quickly, and they may experience difficulty with mobility within 5 to 10 years.
How physical therapy helps
Since PD affects each person differently, our physical therapists partner with you to manage your specific situation — now and as your condition changes. You are not alone! Your treatment plan will be developed after an extensive evaluation by our physical therapists. The examination will include many questions about how your PD affects your life. Special tests will be conducted to examine your posture, strength, flexibility, walking, balance, and coordination.
Our physical therapist will help you stay as active and as independent as possible. You will be taught special exercises and techniques to combat the symptoms of PD. We have a team of physical therapists and a physical therapy assistant that are trained in the LSVT BIG method to help control symptoms and improve your walking and balance. Specifically, this exercise program has shown to increase amplitude of limb and body movement (Bigness) in people with Parkinson’s disease. Research of the LSVT BIG method has shown documented improvements in amplitude (trunk rotation/gait), improved speed (upper/lower limbs), balance, and quality of life. In addition, people are often able to maintain these improvements when challenged with a dual task.
Complex Regional Pain Syndrome (CRPS)
CRPS, formally known as RSD (regional sympathetic dystrophy), is considered to be a multi-system disorder characterized by severe pain; pathological changes of the bones, joints, and skin; excessive sweating; tissue swelling; and hypersensitivity to light touch. CRPS involves the central nervous system, autonomic nervous system, and immune system. Although research has not yet determined exactly why CRPS occurs, physical therapy has proved to be quite beneficial in managing its symptoms, improving function, and increasing the quality of life for people with CRPS.
How physical therapy helps
Physical therapy plays a vital role in the treatment of CRPS. Our physical therapists work with you to develop a treatment plan to help address your individual condition. Since the symptoms of CRPS vary, the approach to care will also vary. CRPS treatment is generally based on the chronicity and severity of the episode. Treatment for CRPS may include movement therapy in which mobilization of the affected body part is done and begins immediately following diagnosis of CRPS. Movement therapy is performed to help prevent contractures (the tightening of muscles or joints) and to maintain function. Physical therapy may include a combination of passive and active movements as well, however, the best treatment for your specific condition will be determined by our physical therapists.
